Our Views
Feasibility study of healthcare centers and hospitals: key considerations
1. Introduction
Feasibility studies play a pivotal role in the planning stages of any project. For a hospital, the stakes are especially high because the outcomes directly impact the health and well-being of a community. A successful feasibility study involves careful analysis, strategic planning, and collaboration among stakeholders to assess the viability of the project from multiple angles.
Hospitals are complex systems requiring significant investment, infrastructure, and skilled personnel. Therefore, the feasibility study must encompass both broad objectives and specific details. It is essential to evaluate the hospital’s potential impact on the community, its alignment with public health priorities, and the practicality of execution.
Key steps include:
- Identifying clear goals and objectives for the hospital project.
- Evaluating the demand for healthcare services in the region.
- Assessing financial, legal, and logistical factors.
- Engaging with local authorities, healthcare professionals, and community members.
- Considering long-term sustainability, including funding and operational plans.
By thoroughly examining these aspects, project planners can build a solid foundation for informed decision-making, ensuring that the hospital project has a meaningful and lasting impact on the community it serves.
A clear vision is the cornerstone of any hospital project. This section sets the direction for the entire feasibility study by answering foundational questions and setting objectives.
2. Defining the Vision
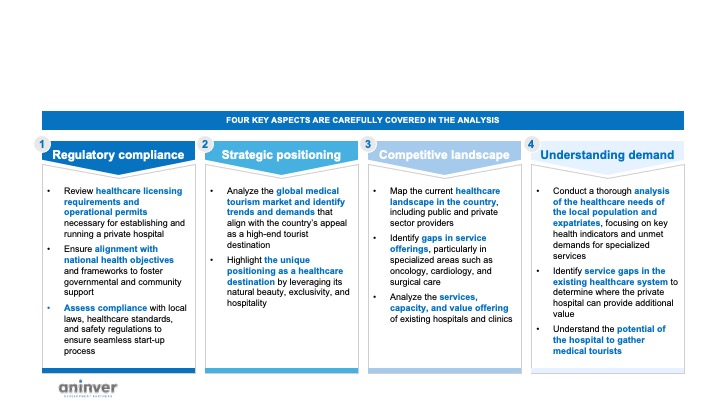
Aspects of a healthcare feasibility study
2.1 Identify the Purpose
Defining the hospital's purpose is crucial to shaping its identity and role within the community. Is the facility intended to provide comprehensive general healthcare, focus on a specific specialty such as oncology or cardiology, or prioritize medical research and education?
For example, a hospital designed to serve a rural area may need to focus on primary care and maternal health, while one in a metropolitan center could emphasize advanced diagnostics and surgical services. Aligning the hospital’s purpose with the community’s needs ensures its relevance and utility.
2.2 Determine the Target Population
The next step involves identifying the population that the hospital will serve. This requires an in-depth understanding of the demographics in the area, including age distribution, income levels, and prevalent health issues. For instance, an aging population may require services like geriatric care and chronic disease management, while a younger demographic might benefit more from maternity and pediatric services.
Estimating the scale of operations is equally important. How many beds will the hospital require? What volume of outpatient services can be realistically expected? By addressing these questions, planners can determine the size and scope of the hospital, which in turn influences decisions about infrastructure, staffing, and financial planning.
2.3 Articulate the Core Objectives
In addition to purpose and population, it is important to articulate broader objectives for the hospital. These might include improving access to healthcare, reducing patient wait times, providing specialized treatments, or creating a hub for medical training and innovation. Clear objectives provide a benchmark against which the success of the project can be measured, ensuring alignment with stakeholders’ expectations.
3. Understanding the Market
Understanding the market is critical to ensuring that the hospital aligns with community needs and operates effectively within the existing healthcare ecosystem. This involves multiple steps:
3.1 Engage Local Stakeholders
Conduct interviews and consultations with local stakeholders, including healthcare providers, community leaders, and government representatives. These discussions provide valuable insights into the region’s specific healthcare challenges, unmet needs, and priorities. Stakeholder input is also essential for building community trust and securing support for the project.
3.2 Analyze Demand Data
Gather and analyze quantitative data to understand the demand for healthcare services in the target area.
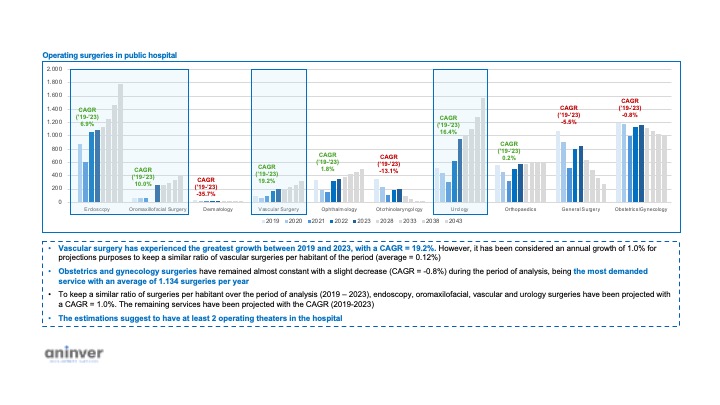
Demand of surgeries
This includes examining population health statistics, disease prevalence, and demographic trends. The analysis should focus on estimating the demand for:
- Outpatient services, including diagnostic tests and consultations.
- Emergency services to handle acute and life-threatening cases.
- Surgical procedures, both routine and specialized.
- The number of hospital beds required based on population size and health trends.
This data ensures that the hospital is designed to meet actual community needs, avoiding overcapacity or service gaps.
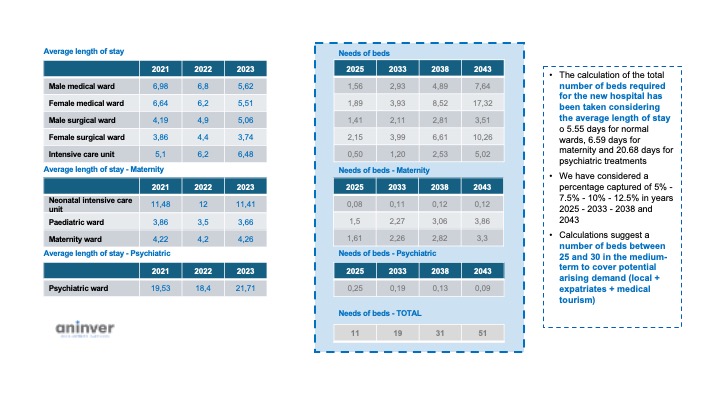
Calculation of number of beds
3.3 Map Healthcare Supply
Develop a comprehensive map of existing healthcare facilities and services in the area. This includes hospitals, clinics, diagnostic centers, and specialist providers. Assess their capacities, service offerings, and geographic reach. By identifying gaps in service provision, planners can determine how the new hospital can complement or enhance the existing system rather than duplicate efforts.
By integrating stakeholder feedback, demand data, and a thorough mapping of the healthcare supply, project planners can ensure that the hospital addresses real community needs and establishes a strong position within the local healthcare landscape.
4. Crunching the Numbers
4.1 Estimate Costs
Developing detailed cost estimates is essential for understanding the financial implications of the project. These estimates should cover:
- Capital Expenditures (CAPEX): Costs for land acquisition, construction, equipment procurement, and initial setup.
- Operational Expenditures (OPEX): Recurring costs such as salaries, utilities, maintenance, and medical supplies.
- Understanding these costs provides a baseline for evaluating the financial requirements and ensuring the project stays within budget.
4.2 Calculate Revenue Projections
Revenue projections should be comprehensive, considering all potential income streams:
- Patient fees for services such as consultations, surgeries, and diagnostics.
- Insurance reimbursements from private insurers and government programs.
- Ancillary income from pharmacies, cafeterias, or parking facilities.
- These projections should reflect realistic utilization rates and price points to avoid overestimations.
4.3 Assess Profitability Metrics
To determine the financial viability of the hospital, use standard profitability metrics:
- Net Present Value (NPV): Evaluate the project’s total expected value over its lifespan, considering the time value of money.
- Internal Rate of Return (IRR): Assess the project’s profitability as a percentage, helping compare it to other investment opportunities.
- Payback Period: Calculate the time needed to recoup the initial investment.
These metrics help stakeholders understand the financial returns and decide whether the project is worth pursuing.
4.4 Perform Sensitivity Analysis
A sensitivity analysis evaluates how changes in key variables impact the project’s financial outcomes. For instance:
- How would a 10% increase in construction costs affect profitability?
- What happens if patient utilization rates are lower than expected?
- How do fluctuations in reimbursement rates influence revenue?
By testing different scenarios, project planners can identify potential risks and develop contingency plans to address them.
5. Choosing the Right Location
Selecting an ideal location for the hospital is a critical decision that impacts its operational efficiency, accessibility, and long-term success. Several factors must be carefully evaluated:
5.1 Evaluate Accessibility
Accessibility is paramount when choosing a site. The hospital should be conveniently reachable for patients, staff, and suppliers. Key considerations include proximity to:
- Major roads and highways to facilitate easy transportation.
- Public transportation options, ensuring accessibility for those without private vehicles.
- Population centers to serve the maximum number of people effectively.
Additionally, planners should evaluate the surrounding infrastructure to ensure smooth patient referrals and supply chain logistics.
5.2 Assess Utilities and Regulations
Adequate utilities are non-negotiable for a hospital. The selected site must have reliable access to:
- Electricity, with backup options to ensure uninterrupted operations.
- Clean water supply and waste management systems.
- High-speed internet for modern healthcare systems and communication.
Moreover, compliance with zoning laws and environmental regulations is essential. An environmental impact assessment should be conducted to ensure the construction and operation of the hospital do not harm the surrounding ecosystem.
5.3 Evaluate Site Conditions
The physical conditions of the site—such as soil quality, topography, and susceptibility to natural disasters—should be assessed. For example, the site must be stable for construction and free from flood or earthquake risks. These factors contribute to both the safety and cost-effectiveness of the project.
6. Navigating Legal and Regulatory Hurdles
Navigating the legal landscape is a crucial part of hospital feasibility planning. Healthcare is a heavily regulated sector, and compliance with legal requirements is essential to avoid delays and potential liabilities.
6.1 Licensing and Accreditation
Ensure that the project complies with all licensing requirements for establishing a hospital. This includes acquiring permits for construction, operation, and service delivery. Accreditation standards must also be met to assure quality care and foster trust among patients and stakeholders.
6.2 Data Privacy and Compliance
Hospitals handle sensitive patient information, making data privacy compliance critical. Adhere to local and international laws governing patient data protection, such as GDPR or HIPAA, depending on the region. Invest in robust IT systems to ensure secure storage and management of patient records.
6.3 Legal Contracting and Partnerships
Review and finalize all legal contracts with partners, suppliers, and contractors. Legal counsel should be engaged to oversee agreements and safeguard the project from potential disputes. Additionally, compliance with labor laws and employee rights must be ensured when hiring staff.
7. Preparing for Risks
Every project comes with risks, and identifying them early allows for proactive management. Hospitals, being complex operations, face a variety of potential challenges:
7.1 Identify Potential Risks
Common risks in hospital projects include:
- Delays in construction due to unforeseen site conditions or regulatory hurdles.
- Cost overruns resulting from inflation, material shortages, or design changes.
- Challenges in recruiting skilled medical and non-medical staff.
- Changes in healthcare regulations that affect the project’s scope or costs.
7.2 Develop Mitigation Strategies
To mitigate these risks, planners can:
- Build contingency funds into the budget to handle unexpected expenses.
- Establish strong project management protocols to ensure timely delivery.
- Develop competitive recruitment and training programs to attract and retain talent.
- Monitor regulatory developments and maintain open communication with authorities to address compliance issues swiftly.
- Proactively addressing risks ensures the project stays on track and within budget, ultimately leading to a successful hospital launch.
Send us a message on our contact page and we can discuss how we can help you.
Some of our experience conducting feasibility studies can be seen below:
- Feasibility study of a private hospital in Seychelles
- Feasibility Study for a new marina in the island of San Andrés through PPP
- Pre-feasibility study for construction of silo storages in Northern Ghana through PPP
- Feasibility study of a real estate WAQF project in Cotonou (Benin)
- Feasibility study and analysis of strategic alternatives of a touristic development in Natal
- Feasibility study for creation of an Investment and Export Promotion Agency of Health services in Tunisia
- Feasibility Study for car parks in Bishkek though PPP
- Feasibility study of markets in Benin and Togo under PPP scheme
- Feasibility Study for the establishment of a Large-Scale Cashew Processing Plant in Zambia
- Public Private Partnership (PPPs) study in the Housing Sector
- Review of Business Case for Manila Central Subway
- First Mover PPP Prefeasibility Study
- Review of the feasibility study of the PPP project Complejo El Brillante, in Cordoba (Spain)
- Review of pre-feasibility study of a Health PPP project